“Good ideas are not adopted automatically. They must be driven into practice with courageous patience.” - Hyman Rickmore
As an integral cornerstone of societal infrastructure, energy systems underpin our daily activities and catalyze the evolution of our civilization. It has long been axiomatic that energy demand and GDP growth are correlated. When economies grow, their energy consumption/demand increases. If access to energy becomes constrained, GDP growth pulls back.
However, during my time as a college student in Austin, I have been witness to, and affected by, two total grid failures, supplemented by numerous power outages over a span of four years.
To understand the broader context of these issues, how they came to be, and the grid inter-workings in general, it is essential to understand the concept of the “three-legged stool” of energy: production, delivery, and consumption. For the system to work effectively, each leg must be robust and in balance.
Production: The generation and extraction of energy.
Delivery: The moving of power from where it is generated to where it is consumed.
Consumption: The demand side of energy, encompassing how energy is utilized by end-users, including households, industries, and services.
Difficulties with the grid predominantly originate from challenges in the delivery. The production aspect is largely influenced by incentive structures associated with renewable & nonrenewable sources, while consumption is driven by demand. These elements significantly impact the grid's proficiency in energy transmission (delivering), but are far from the core of what the grid does.
Breaking Down the Issue
As mentioned, the core issue can be examined using the three-legged stool framework. This reveals a misaligned incentive model, caused by regulations implemented over the past century, and an absence of basic innovation.
Production
The push for clean energy and increased electrification of the world has led to a growth in variable sources of energy.
Diversification of Energy (Increased Cost & Volatility): The emphasis on developing and deploying affordable clean energy sources has resulted in technological advancements. These have made variable sources like solar and wind more cost-effective. However, according to IREA, while solar has become the cheapest source of new electricity generation, it has also complicated energy delivery as a result of increased peak-trough volatility. The variability requires more sophisticated grid management and storage solutions for delivery.
Delivery
The process of delivery has become increasingly challenging due to several factors:
Aging Infrastructure: Much of the current transmission and distribution infrastructure is outdated and in need of upgrades or replacement. This aging infrastructure is less capable of handling the dynamic demands of modern electricity delivery, especially with the integration of more variable and distributed energy sources.
Grid Reliability: The reliability of the grid has been declining, not only because of the growing use of renewables but also due to increased frequency of extreme weather events and insufficient maintenance of distribution systems. These issues have resulted in more frequent and severe outages (U.S. Department of Energy, 2021).
Increasing Costs: As the demand for electricity grows, driven by trends such as the electrification of transportation and heating, the costs associated with delivering power to consumers have risen. This is partly because transmission lines must be sized to handle peak loads, even if those peaks occur infrequently.
Regulatory and Permitting Delays: Modernizing the grid is hindered by regulatory and permitting challenges. For example, building new transmission lines often faces significant delays due to the need for approvals across multiple jurisdictions and the complexities of land acquisition.
Consumption
As mentioned, there is an increasing effort to electrify as much of the economy as possible. While these changes are crucial for reducing greenhouse gas emissions, they also increase the demand for electricity and the complexity of managing grid loads.
Consumption Patterns: As consumption patterns evolve, the grid must adapt to these new loads. For instance, electric vehicles create new demand peaks.
History of the Grid
To better comprehend the issues at hand, it is crucial to review the extensive history of the grid and its influence on its current state. However, because the information is detailed, it may be beneficial to quickly go through it, skim the text, and examine the diagrams.
The historical context of grid information was largely obtained from the excellent four-part substack by Construction Physics, along with other reputable sources.
Early History
In the early 20th century, U.S. electricity was a luxury, used by less than 5% of industries and 8% of homes. Today, it's a widespread utility, with over 89% of the global population having access, increasing to 97% in urban areas. The modern electrical grid's inception can be traced back to Edison's invention of the incandescent light bulb in 1879. This innovation replaced gas lighting, which was labor-intensive and provided insufficient illumination. Early electric lighting technologies, such as arc lamps (1858), were unsuitable for domestic use due to their intense brightness. Edison developed a practical incandescent lamp by heating a resistive material. His design, which reduced copper use in wiring, made electrical lighting affordable, leading to over 1,100 central power stations by 1891.
Currents: AC & DC
Edison's direct current (DC) was inefficient for long-distance power supply due to significant power loss as heat in wires. Just like water in a pipe, where current is the water flow and voltage is the pressure, high current at low voltage leads to substantial losses over distance.
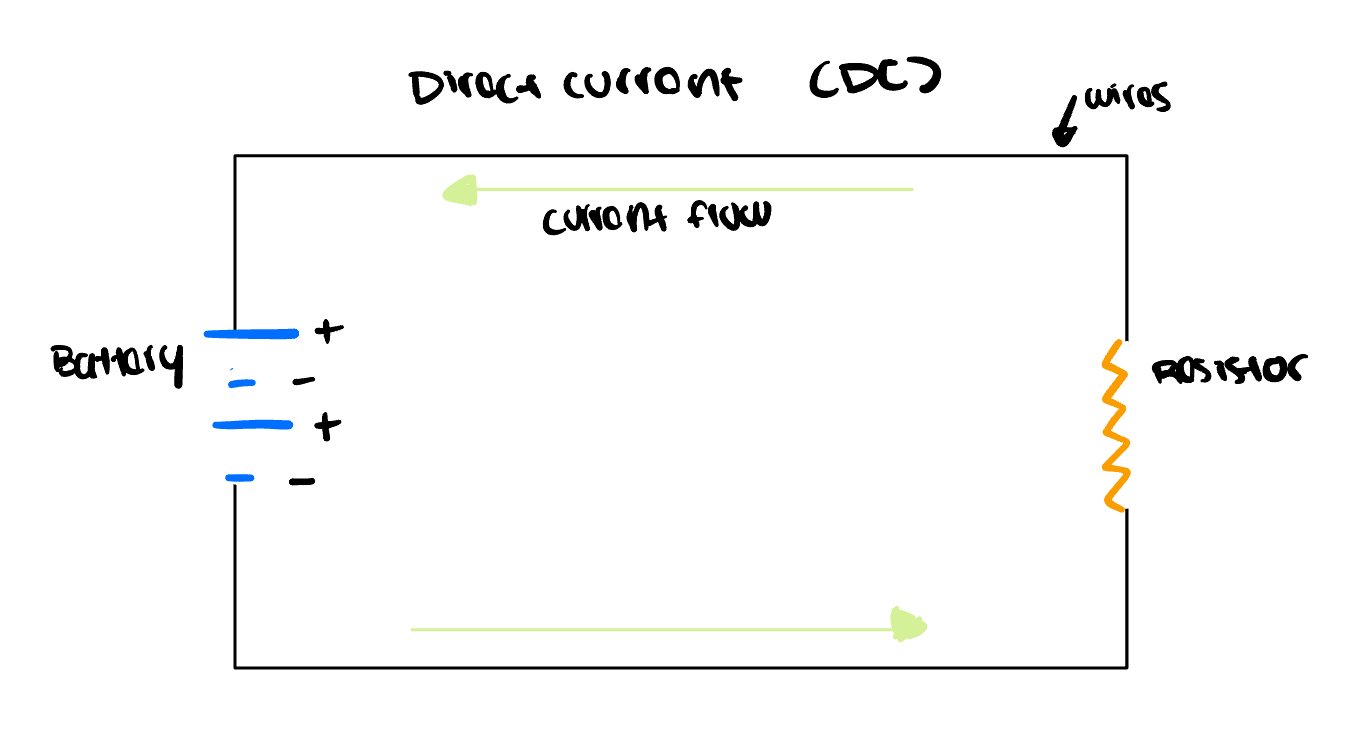
A DC (Direct Current) circuit operates through the interplay of several key components. The battery serves as the power source, with current exiting its positive (+) terminal and returning to its negative (-) terminal. Wires connect the battery to other components, creating a closed loop for current to flow. Within this loop, a resistor often plays a crucial role by limiting the amount of current and protecting other components from excessive flow. The current in a DC circuit follows a consistent direction, moving from the battery's positive terminal, through the wires and components like the resistor, and back to the negative terminal.
Resistor (Limits Current): The resistor restricts the amount of current flowing through the circuit, helping to protect other components from excessive current
In contrast, alternating current (AC) offered a solution. AC systems, championed by Nikola Tesla and backed by George Westinghouse, used transformers to step up the voltage for long-distance transmission and then step it down for local use. This allowed power to be transmitted over much longer distances without significant losses, making it more suitable for widespread distribution.
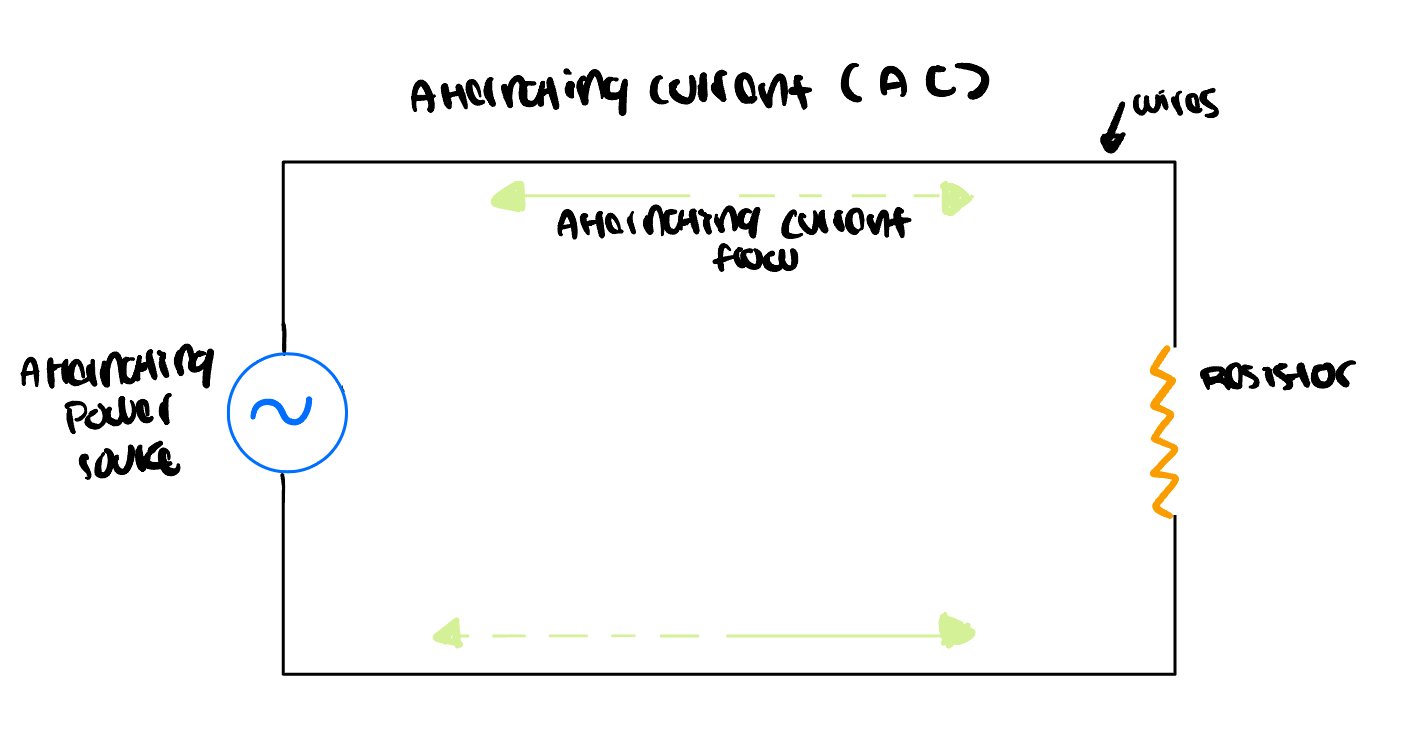
An AC (Alternating Current) circuit is powered by an alternating power source, typically referred to as an AC supply. Unlike DC circuits, the current in an AC circuit periodically changes direction, usually in a sinusoidal waveform. This means the flow of electricity reverses its direction many times per second (e.g., 50 or 60 times per second in most household systems). Wires serve as the current path, connecting the AC supply to other circuit components and forming a loop for the current to travel. A resistor is often included to limit and control the current flow, protecting other components from excessive current. The alternating nature of the current is a defining feature of AC circuits, with electrons moving back and forth rather than in a constant direction. This back-and-forth movement of current allows for efficient long-distance power transmission and is the standard for household and industrial electrical systems worldwide. The ability to easily transform voltage levels using transformers is a key advantage of AC systems, enabling the high-voltage transmission and lower-voltage distribution that characterizes modern power grids.
Despite Edison’s resistance and his campaign against AC’s safety, AC technology eventually prevailed. The ability to convert between AC and DC using devices like the rotary converter, invented by Charles Bradley in 1888, allowed both systems to coexist initially. By 1917, AC had become the dominant method for electrical transmission, with 95% of power stations generating AC.
An AC to DC converter, also known as a rectifier, transforms alternating current (AC) from a power source like a wall socket into direct current (DC) for use in electronic devices. The process begins at the AC input, where the alternating current enters the circuit. A ground connection is incorporated for safety, providing a path for excess charge to dissipate into the earth. The incoming AC then passes through a transformer, which adjusts the voltage to the desired level by either stepping it up or down. Next, a bridge rectifier, typically composed of four diodes, converts the AC into pulsating DC by allowing current to flow in only one direction. However, this pulsating DC isn't smooth enough for most applications, so a filter capacitor is employed to smooth out the voltage fluctuations, acting like a reservoir that fills during voltage peaks and discharges during troughs. The result is a steady DC output suitable for powering various electronic devices and components. This conversion process is crucial for many modern electronics that require DC power but are plugged into AC outlets.
While a comprehensive understanding of AC to DC transformers or the specifics of AC and DC currents might not be necessary unless you're an engineer, it's still important to have a basic grasp of these concepts. These principles are frequently referenced in discussions around electricity, and understanding them can provide valuable context.
The Grid Today & Regulatory Dynamics
Post the 1930s, regulatory dynamics began to shape the formation of the grid. To clarify terminology from the outset, here are all the key regulatory bodies and other noted key players that play a significant role in the grid and its dynamics.
Independent System Operators (ISOs): Organizations that coordinate, control, and monitor the operation of the electrical power system within a specific region. They ensure the reliable delivery of electricity, maintain balance between supply and demand, and oversee electricity transactions.
Regional Transmission Organizations (RTOs): Entities similar to ISO but typically cover larger geographical areas. They coordinate, control, and manage high-voltage electricity transmission networks across multiple states or countries. They are responsible for ensuring the efficient and reliable delivery of electricity to vast regions.
Federal Energy Regulatory Commission (FERC): FERC plays a central role in overseeing the interstate transmission of electricity, natural gas, and oil. It regulates the wholesale electricity markets and ensures fair competition by overseeing the activities of Independent System Operators (ISOs) and Regional Transmission Organizations (RTOs). FERC's regulatory purview includes approving tariffs and setting rates for transmission services, ensuring that these rates are just and reasonable.
State Public Utility Commissions (PUCs): At the state level, Public Utility Commissions are responsible for regulating retail electricity rates and services within their respective states. PUCs oversee the operations of investor-owned utilities (IOUs) and, in some states, have a role in guiding the implementation of renewable energy policies and energy efficiency programs.
Environmental Protection Agency (EPA): The EPA's regulations impact the energy sector significantly, particularly through policies related to emissions and environmental compliance. Regulations such as the Clean Air Act and the Clean Power Plan (though legally challenged and evolving) influence the types of power generation that are economically viable and encourage shifts towards cleaner energy sources.
Department of Energy (DOE): The DOE provides policy guidance, research funding, and support for energy innovation. It plays a critical role in advancing technologies that enhance energy efficiency, grid reliability, and the integration of renewable energy sources.
North American Electric Reliability Corporation (NERC): NERC is responsible for developing and enforcing reliability standards for the bulk power system. It ensures that the U.S. electric grid operates reliably and securely, especially as the grid incorporates more variable renewable energy sources.
The Expansion of the Grid (1930 - Present)
By 1930, the U.S. consumed around 114 billion kilowatt-hours of electricity annually, generated by over 40,000 power plants. Coal-fired plants produced 56% of this, while hydroelectric power contributed 34%. The New Deal in the 1930s expanded and regulated electricity production and distribution, notable projects included the Hoover Dam and the establishment of the Rural Electrification Administration (REA). After the 1929 crash revealed the precariousness of utility empires like Samuel Insull's, stringent regulation was imposed on utility holding companies through the Public Utility Holding Company Act (PUHCA) and the Federal Power Act.
The post-World War II period saw a surge in electricity demand and a corresponding expansion in generating capacity. Between 1940 and 1945, U.S. electricity consumption increased by 60%, even as generation capacity only rose by 25%. This period highlighted the efficiencies gained through the interconnection of regional power grids, which not only facilitated capacity expansion but also enhanced the system's resilience to potential disruptions. By the 1960s, the U.S. electric power industry had become the largest by asset value, surpassing even the next two largest industries combined. During this time, the country utilized more than 40% of the world's electric power, despite global advances in electrification. The construction of nearly 80,000 miles of transmission lines from 1950 to 1963 exemplified the scale of infrastructure development required to meet this demand. Most power providers had integrated their systems into a few large, interconnected networks, enhancing operational efficiency and reliability.
However, the industry's rapid growth began to show signs of strain by the late 1960s. The environmental movement, bolstered by the National Environmental Policy Act (NEPA) of 1969, imposed new constraints on infrastructure projects. Additionally, the rising costs and safety concerns associated with nuclear power plants, which had been heavily promoted as a future energy source, further complicated the industry's expansion strategies.
The 1970s marked a period of significant upheaval for the U.S. electricity industry. The 1965 Northeast blackout, which left 30 million people without power for up to 13 hours, exposed the vulnerabilities of a highly interconnected power system. The ambitious Golden Spike Operation of 1967, which attempted to link the U.S. power grid into a single system, ultimately failed due to instability, leading to the removal of AC ties and the adoption of high-voltage DC transmission lines for inter-grid power sharing.
The energy crisis of 1973 exacerbated these challenges, causing demand growth to plummet and electricity prices to skyrocket by nearly 390% in real terms between 1973 and 1983. This period saw the introduction of significant legislative measures aimed at restructuring the industry. The Public Utility Regulatory Policies Act (PURPA) of 1978, part of the National Energy Act, mandated utilities to purchase power from non-utility producers at a rate equivalent to the utility's avoided cost. This policy fostered the emergence of Independent Power Producers (IPPs) and set the stage for greater competition in power generation.
In response to escalating costs and the inefficiencies of the existing system, the Federal Energy Regulatory Commission (FERC) began restructuring the industry in the mid-1980s to introduce competitive market principles. The Energy Policy Act of 1992 further facilitated this transition by creating a new class of power suppliers, the Exempt Wholesale Generators (EWGs), who could sell power without being regulated as utilities. This act also mandated the establishment of Independent System Operators (ISOs) to manage transmission lines and wholesale power markets, aiming to reduce costs and enhance market competition.
The deregulation efforts of the 1990s culminated in a mixed legacy. The FERC's initiatives to create competitive wholesale electricity markets led to the formation of Regional Transmission Organizations (RTOs), which assumed broader responsibilities for system reliability and market operations over wide geographic areas. However, the implementation of deregulation faced significant challenges, most notably in California.
In California, market design flaws and regulatory constraints led to a severe energy crisis in 2000-2001. Wholesale electricity prices soared, driven by market manipulations by companies like Enron, which exploited the system's vulnerabilities. Utilities, unable to pass on the increased costs to consumers due to rate caps, faced financial ruin, resulting in widespread blackouts and a collapse of public confidence in deregulated markets.
Despite these setbacks, deregulation persisted in various forms across the U.S. Today, approximately two-thirds of the country's electricity is supplied through ISO/RTO-managed markets, while the remaining third is provided by traditional vertically integrated (the chain of production to delivery is owned by utility companies) utilities. The industry continues to grapple with the balance between market competition and regulatory oversight, as it navigates the challenges of modern energy demands and the transition to more sustainable sources.
The regulatory architecture that dominates the U.S. energy industry today is a complex and multifaceted construct, engineered to harmonize various interests. These range from guaranteeing a reliable supply of power and safeguarding consumers, to promoting competition and facilitating the shift towards renewable energy. For a more nuanced understanding of the operational differences between regulated and deregulated markets, I will delve into this in the subsequent section. This information is instrumental in devising solutions for the identified issues within the "three-legged stool" framework previously discussed.
Regulated vs. Deregulated Markets
Regulated and deregulated markets significantly impact the delivery of power to end consumers. The aim of deregulation is to enhance competition, which in turn reduces costs for the end user. However, this does not always work well in practice. In a deregulated structure, retail customers can select their electricity suppliers. Meanwhile, utilities must sell off their generation assets and purchase electricity from a new wholesale market. The key players in this process can be confusing, and I believe they can be better explained through the diagram below.
Energy Producer: Companies or entities that generate electricity from various sources like coal, natural gas, nuclear, hydro, wind, or solar power. In regulated markets, the energy producer tends to be monopolized and owned by the utility companies. Produce electricity that is then sold to utility companies for distribution to consumers.
Utility Company: A company that manages the entire process of producing, transmitting, and distributing electricity to consumers. Responsible for generating electricity, transmitting it through high-voltage power lines, and distributing it to end customers. Operates as a regulated monopoly under state supervision.
Distribution Network: The network of lower-voltage power lines that deliver electricity from substations to homes and businesses. Transports electricity from the utility company’s transmission system to end customers.
State Public Utility Commission (PUC): A state-level regulatory body that oversees the operations of utility companies. Regulates utility companies to ensure reliable service, fair pricing, and compliance with state laws.
Wholesale Market: A market where large quantities of electricity are bought and sold between producers and entities like utility companies or retail suppliers. Facilitates the trading of electricity among producers, utilities, and suppliers to balance supply and demand.
Retail Supplier: Companies that purchase electricity from the wholesale market and sell it to end customers. Compete with other suppliers to provide electricity to consumers, offering various pricing plans and services.
One More Thing: Supply-Demand Peaks & Troughs
This is one concept that I think is crucial to understand the underlying reasons for issues with the grid, but I was stuck one where to stick it in. Supply-Demand Peaks & Troughs are a crucial concept to understand the management of electricity grids.
Peaks: These are periods when electricity demand is at its highest. Peaks often occur during specific times of the day, typically in the morning when people wake up and start their daily activities, and in the evening when they return home and use household appliances.
Troughs: These are times when electricity demand drops to its lowest levels. Troughs usually happen late at night or early in the morning when most people are asleep, and industrial activities are minimal. This can be signified through terms such as the “Base Load.”
As mentioned, electricity providers must constantly adjust the supply to match these demand fluctuations. This dynamic balancing act involves various components and strategies within the power grid system. Excessive demand during peak times can push the grid beyond its supply capacity, risking overloading and potential damage to the system. To mitigate this risk, grid operators may implement load-shedding measures or reduce voltage (brownouts) to balance the load. Conversely, insufficient supply can occur due to failures at power plants, faults in transmission lines, or fuel shortages, leading to power outages if the available electricity does not meet the demand.
However, electricity demand does not remain constant throughout the day. It fluctuates, with significant increases during peak times, such as in the mornings and evenings when people are most active, and drops to its lowest during the late night and early morning hours. These fluctuations are addressed by peaking power plants, which can quickly ramp up or down their electricity production to meet sudden spikes in demand. The integration of renewable energy sources, such as solar and wind, adds another layer of complexity due to their intermittent nature.
Solutions
With a comprehensive understanding of the historical context, grid structure, and market dynamics, we can now focus on potential solutions to the challenges faced by the electricity grid. These challenges are predominantly in delivery, significantly impacted by the increase in variable energy sources and inconsistent energy demand.
Stabilizing Production
Although the focus here is on delivery, here are a few solutions for production. This is a highly contentious issue, with an ongoing debate about how best to generate electricity sustainably. Renewable energy sources like wind and solar, while environmentally friendly, add volatility to the grid due to their intermittent nature. To mitigate this, investing in grid-scale energy storage solutions is crucial. Technologies such as lithium-ion batteries, flow batteries, and hydrogen storage can store excess energy produced during peak generation times and release it during periods of high demand or low generation. This capacity to balance the supply and demand fluctuations of renewables helps stabilize the grid.
On the nuclear front, modern small modular reactors (SMRs) represent a promising development. These reactors are designed to be safer and more flexible than traditional large reactors and can provide a reliable, low-carbon baseload energy source. Easing regulatory restrictions and providing incentives for nuclear development could significantly enhance energy security and provide consistent power that complements the variability of renewable energy sources.
Additionally, encouraging the adoption of Distributed Energy Resources (DERs), such as rooftop solar panels and micro wind turbines, can reduce the load on centralized power plants and minimize transmission losses. These small-scale, local generation technologies can be integrated into the grid through smart inverters and managed to optimize energy flows and enhance resilience. By generating electricity closer to where it is used, DERs contribute to a more robust and decentralized energy system.
Modernizing Delivery Infrastructure
The next set of solutions focuses on improving the delivery infrastructure. The aging transmission and distribution systems need substantial investment to replace outdated components like old power lines, substations, and transformers with modern, more resilient equipment. This is especially critical because a significant portion of grid failures occur within the distribution system, the low-voltage network that directly delivers electricity to consumers. In the United States, most distribution lines are mounted on poles and are vulnerable to weather-related disruptions, such as high winds, ice, and extreme heat. In contrast, countries like Germany have buried a large percentage of their distribution lines, protecting them from such conditions.
Integrating advanced technologies into the grid can also enhance its responsiveness and reliability. Smart meters and real-time monitoring systems allow utilities to quickly identify and resolve issues, minimizing downtime during outages. Advanced grid management software can optimize electricity flow, integrating data from various sources to predict demand, manage energy flows, and coordinate with DERs. This is essential for effectively managing the complexities introduced by the increasing presence of variable renewable energy sources.
Expanding the deployment of energy storage systems at both the grid-scale and consumer levels is another crucial step. Large-scale storage solutions, such as lithium-ion batteries and pumped hydro storage, can act as buffers, absorbing excess energy during periods of high production and releasing it when demand increases or generation decreases. This not only stabilizes the grid but also reduces the need for additional peaking power plants and minimizes transmission losses. On the consumer level, home batteries paired with solar panels provide a backup power source during outages and enable participation in demand response programs, thus enhancing grid reliability and reducing dependence on the central grid. Emerging technologies like hydrogen storage and compressed air energy storage offer promising solutions for long-duration storage, complementing the quick response capabilities of batteries.
Finally, promoting the development of microgrids and community-based energy projects can enhance local resilience and reduce reliance on centralized power systems. Microgrids can operate independently of the main grid, ensuring a continuous power supply during outages and proving particularly valuable in disaster-prone or remote areas. Community energy projects, such as neighborhood solar farms, allow for collective investment in local renewable generation and shared storage, lowering costs and fostering community involvement in energy management. These projects also contribute to overall grid stability by providing ancillary services like frequency regulation and voltage support. To encourage their development, regulatory support and financial incentives are necessary. Simplifying interconnection processes and establishing clear policies for shared energy savings can accelerate their adoption, creating a more resilient, sustainable, and decentralized energy system that empowers communities and enhances overall grid stability.